It’s vital to keep in mind that vocal cord dysfunction and asthma can coexist, complicating diagnosis. If you or someone you know has a suspicion of vocal cord dysfunction, tell your doctor, who may refer you to a pulmonologist to examine your breathing or an ENT to evaluate your voice cords. Finally, you’ll need to identify a speech pathologist who has worked with vocal cord dysfunction before.
Table of Contents
What is vocal cord dysfunction (VCD)?
Vocal Cord Dysfunction is a condition in which your vocal cords do not work properly. Paradoxical vocal fold motion disorder is another name for it. When you breathe in and out with VCD, your voice chords open instead of closing. VCD is an upper airway illness caused by irritation of the voice box. It is a kind of irritable larynx syndrome.
What do you mean by vocal cords and what is the role of vocal cord?
Your vocal chords are located deep within your voice box in your throat (larynx). When you breathe in (inhale), your voice cords normally open. This allows air to enter your lungs and windpipe (trachea). Your vocal cords open and release the air out of your lungs when you exhale (breathe out). Breathing out causes your vocal cords to vibrate, allowing you to generate speech sounds.
Your vocal cords close while you speak. It’s easier to speak when your vocal cords close.
It is more difficult to get air into or out of your lungs.
Vocal cord dysfunction: Is it a type of asthma?
Breathing can be difficult due to asthma or vocal cord dysfunction. Coughing, wheezing, throat tightness, and hoarseness are all signs and symptoms of both conditions, but they’re not the same thing. But unfortunately vocal cord dysfunction in not a type of asthma.
Asthma Symptoms includes:
- Breathing problems.
- Coughing, which occurs more frequently during colds, activity, at night, or in response to other stimuli.
- Exhalation causes wheezing.
- Tightness in the chest
- Asthma rescue therapy provides relief (inhalers).
Difference between Vocal Cord Dysfunction and Asthma :
| Vocal Cord Dysfunction | Asthma |
| Symptoms appear soon after you start exercising. | Symptoms appear later in the workout process. |
| Throat constriction. | A feeling of tightness in the centre or lower chest. |
| Inhaling is difficult. | Exhaling is difficult. |
| Hoarseness. | There is no hoarseness. |
| The albuterol inhaler has no effect on the symptoms. | Symptoms are controlled by using an albuterol inhaler. |
| Symptoms return almost quickly after stopping Albuterol medication. | When exercise is resumed following Albuterol medication, the symptoms are less severe. |
| The time it takes to recover is less than ten minutes. | Without medicine, recovery can take up to an hour. |
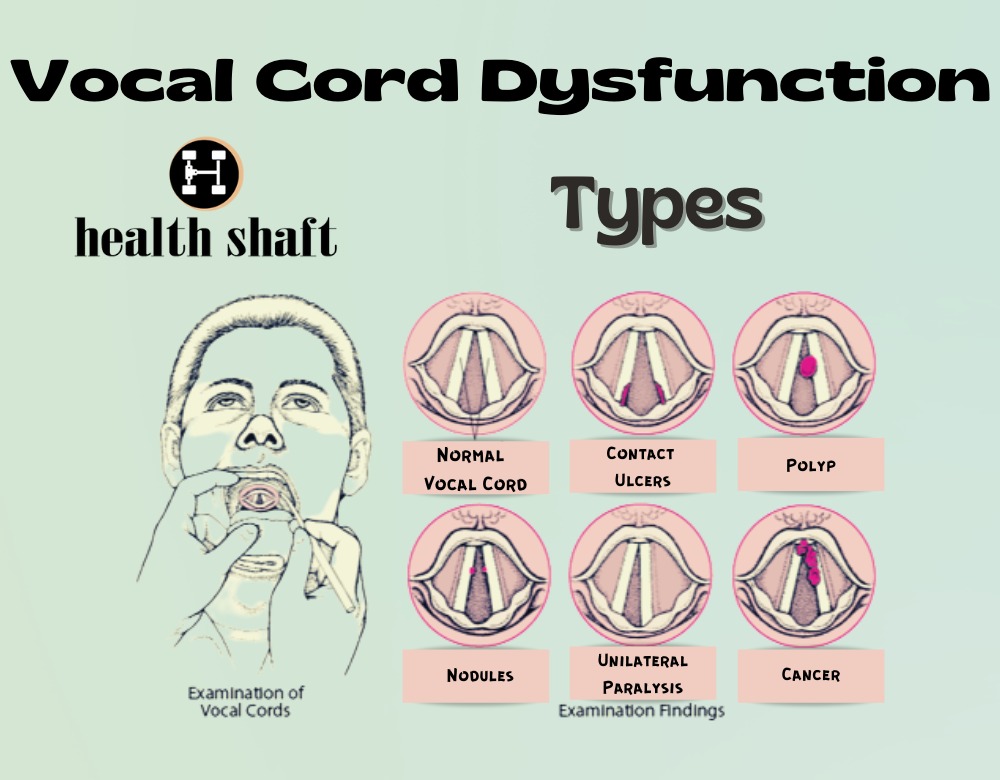
Types of vocal cord dysfunction (vocal cord disorder)
Some common vocal cord disorders types are:
Laryngitis
Your vocal cords are two folds of mucous membrane that cover muscle and cartilage inside the larynx. Your vocal chords open and close smoothly in normal circumstances, generating sounds with their movement and vibration.
Vocal Nodules
Voice nodules are noncancerous growths on your vocal cords that are firm and harsh. They can range in size from a pinhead to a pea.
Under a microscope, vocal cord nodules resemble calluses and are occasionally accompanied with aberrant blood vessels. Vocal cord nodules are more common in women between the ages of 20 and 50, but they can afflict both men and women.
You get nodules when you strain or overuse your voice, such as when you sing, yell, or talk loudly or for a long time. Vocal nodules are known by a variety of names depending on their cause. “Singing nodules,” “screamer’s nodules,” and “teacher’s nodules” are some of the names given to them.
Vocal Polyps
Polyps can develop on either one or both vocal folds. They can resemble a bloated lump, a blister, or a long, thin growth. The majority of polyps are larger than nodules, which means they have more blood vessels and have a reddish appearance. They’re also known as polypoid degeneration or Reinke’s edoema. A nodule can be thought of as a callous, and a polyp as a blister.
Vocal Cord Paralysis
The vocal folds are two elastic bands of muscular tissue found right above the trachea (windpipe) in the larynx (voice box) .Your vocal folds stay apart when you breathe and close tightly when you swallow. When you speak, however, the air in your lungs causes your vocal folds to vibrate back and forth between open and closed states.
Vocal cord paralysis occurs when nerve impulses to the voice box (larynx) are disrupted. As a result, the muscles of the voice chords become paralysed.
Vocal cord paralysis can make it difficult to speak and even breathe.
That’s because your vocal cords, also known as vocal folds, are responsible for more than just sound production.
The condition of a single vocal cord paralysis is far more common than that of a double vocal cord paralysis. The illness can affect people of all ages and genders. Women, on the other hand, are more prone than men to suffer from vocal cord paralysis. Both vocal chords becoming paralyzed is a rare occurrence.
What are the symptoms of vocal cord dysfunction?
You may not have any symptoms if an acute episode is minor.
Exercise is the most common cause of VCD. Shortness of breath, throat tightness, and loud breathing are common symptoms of the affected person (stridor). Dizziness may occur if the symptoms persist for many minutes.
When you do experience symptoms, it’s usually due to inhaled air passing through a smaller region than typical. They appear out of nowhere and can be mistaken for an asthma attack.
Vocal Cord Dysfunction Symptoms includes:
- Breathing problems.
- During episodes, there is coughing.
- Breathing that is too loud (most often high pitched whistling sound with inhalation).
- Tightness in the neck, throat, or upper chest.
- During or after an episode, you may have a hoarse voice or have difficulty speaking.
- Medications for asthma do not help to alleviate symptoms.
Primary treatment of VCD speech therapy
The most common treatment for vocal cord disorder is VCD speech therapy. To acquire breathing techniques to control VCD, the patient will normally need to attend three to four speech therapy sessions.
The patient may be asked to run on a treadmill during these sessions in order to elicit VCD symptoms. To help relax the muscles of the throat, relaxation exercises are also given.
Another crucial aspect of treatment is supportive counseling. Counseling might assist a VCD patient in adjusting to their diagnosis and treatment plan. It can also assist the individual in recognizing and dealing effectively with stress, which may be a contributing factor in VCD.
Treatment of vocal cord dysfunction
VCD is usually treated with activities that relax the throat muscles. Whether you have an acute (severe) episode of vocal cord dysfunction or not will determine the treatment you receive. During an episode, you may receive the following treatments:
- Speech therapy
- Deep breathing techniques
- Heliox
- Tracheostomy
- Dealing with the cause of the episode
- Psychotherapy
The goals of this treatment of vocal cord dysfunction sessions are to:
- Sources of chronic throat irritation should be identified and eliminated.
- Identify and control PVFM episode triggers.
- Provide an exercise programmed to help patients gain better control over their breathing, minimize the discomfort and fear associated with shortness of breath, and reduce the frequency and duration of PVFM episodes.
- Include comments to assist the person in learning to relax their throat and maintain their vocal cords apart while breathing.
Vocal cord dysfunction breathing exercises
A rescue breath is a breathing practice for VCD. Begin with your lips pursed for this exercise (tightly together).
Exhale slowly and deeply through your pursed lips. Then, through your nose, take two short inhales.
Repeat this breathing pattern a few times until you notice an improvement in your breathing. You should practice this exercise even if you are not having a VCD attack because it is an exercise you can try if you feel a VCD attack coming on.
Vocal Cord Dysfunction Breathing Exercises are as follows:
Diaphragmatic breathing or Belly Breathing
When breathing, diaphragmatic breathing (sometimes known as “belly breathing”) requires fully activating the stomach, abdominal muscles, and diaphragm. With each inward breath, you must deliberately pull the diaphragm down. In this approach, diaphragmatic breathing aids in the efficient filling of the lungs.
How to do this VCD breathing exercise:
- Sit in a way that permits your neck and shoulders to relax while maintaining a straight back.
- Put your hand on stomach. Inhale slowly and deeply with the help of your nose, pushing your palm outside from your body.
- Place the tip of your tongue where your upper teeth meet the roof of your mouth as you begin to exhale. As you exhale, you’ll be able to make a hissing or “S” sound. Back pressure is created, which helps to maintain the airway open.
- Slowly exhale, allowing your hand and belly to glide inward to a resting posture, and hiss or produce a “S” sound as you push air between your tongue and teeth.
- Repeat 10 repetitions and practice 3 times a day so you’ll be ready when VCD strikes.
Paused breathing Exercise
How to practice this VCD breathing exercise:
- Sit in a position that allows you to relax your neck and shoulders while keeping your back straight.
- Inhale slowly and deeply through your nose.
- Exhale by sticking your tongue out of your mouth, beyond your teeth and bottom lip. This forward tongue stretch aids in the opening of the vocal cords’ airway. With a strong spasm, this may be tough at first, but it will become easier as you practice.
- Exhale only through the lips in slow, stopped, or spaced breaths with the tongue out. The timing should be like saying Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha, Ha Don’t use your voice; simply exhale.
- Repeat 10 repetitions and practice 3 times a day so you’ll be prepared if VCD strikes.
People for Ask
Is vocal cord dysfunction life threatening?
Although vocal cord dysfunction is rarely life-threatening, its distressing symptoms can cause patients to be afraid of their next attack and avoid exercising completely, significantly impacting their emotional and physical health.
Most people only experience VCD episodes every now and again, with just modest symptoms. Others have more severe episodes or have them more frequently.
How do you treat vocal cord dysfunction?
The most common non-medicinal treatment for vocal cord dysfunction is respiratory retraining therapy with a skilled speech-language pathologist. Two to six 60-minute sessions are usually required for therapy. Identify and eliminate sources of chronic throat inflammation throughout these sessions.
Identify and control PVFM episode triggers.
Provide an exercise programmed to help patients gain better control over their breathing, minimize the discomfort and fear associated with shortness of breath, and reduce the frequency and duration of PVFM episodes.
Include comments to assist the person in learning to relax their throat and maintain their vocal cords apart while breathing.
What is the best treatment for vocal cord dysfunction?
Speech therapy is primary and best treatment for vocal cord dysfunction. Exercises meant to relieve VCD episodes are taught to you by specially qualified speech-language pathologists. To control episodes of breathing difficulty, you’ll master relaxed-throat breathing and lower-abdominal breathing practices.
Do I have VCD or asthma?
When you breathe in or out, your voice cords close abnormally. This is known as vocal cord disorder. Laryngeal dysfunction, paradoxical vocal cord movement disorder, or paradoxical vocal fold motion are all terms used to describe this condition. Breathing in lung irritants, having an upper respiratory illness, or exercising can all cause vocal cord disorder.
Vocal cord dysfunction, unlike asthma, is not an immune system reaction and does not affect the lower airways. The treatments for the two illnesses are also distinct.
If you have any of the following symptoms, your doctor may consider vocal cord dysfunction rather than asthma:
When symptoms flare up, breathing in is more difficult than breathing out.
Medications for asthma don’t seem to be helping you.
Do inhalers help vocal cord dysfunction?
Inhalers such as Albuterol or inhaled steroids do not treat VCD because it is not a respiratory issue. VCD is usually treated with a series of breathing exercises aimed at retraining the voice cords to relax during breathing and encouraging the patient to use the diaphragm, a muscle in the abdomen.
Conclusion
To avoid misdiagnosis and mismanagement of asthma, early detection and treatment of VCD is critical. Furthermore, vocal cord dysfunction and asthma can coexist. VCD’s origin and path physiology need to be better understood.
A severe episode of VCD can be frightening since you feel and sound as though you are unable to breathe. The best thing you can do is prepare by learning relaxation techniques for your vocal cords, body, and mind. These methods can help you cut down on the amount of episodes you have and even stop them.