Table of Contents
Pneumonia meaning
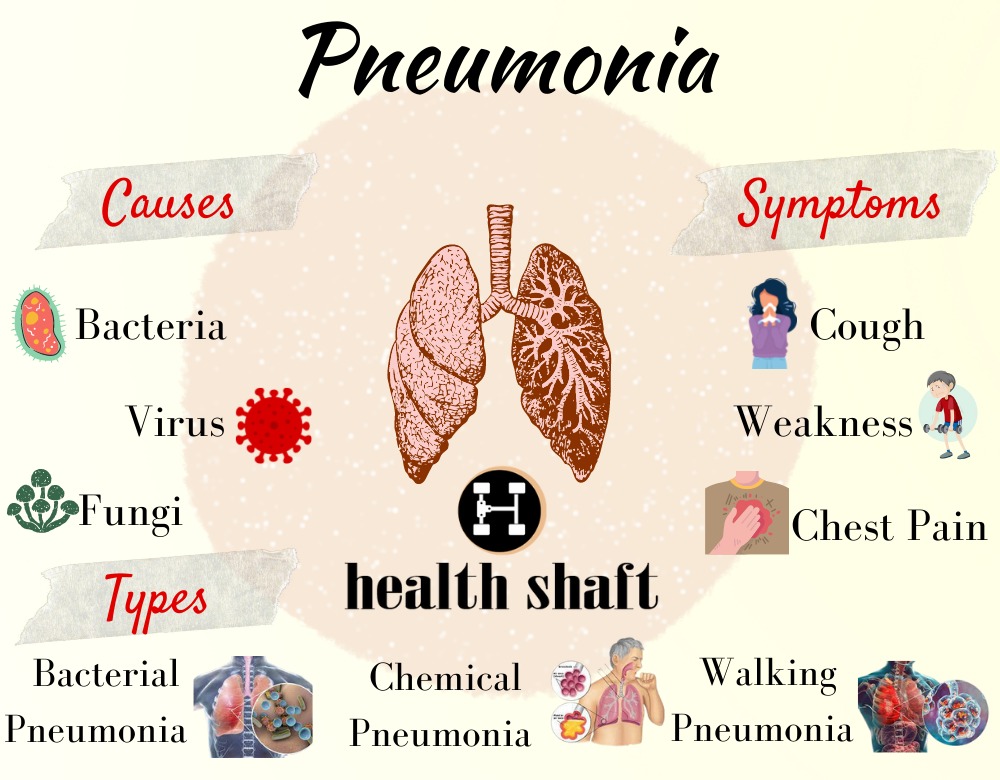
Pneumonia is a bacterial, viral, or fungal infection of one or both lungs. Inflammation of the alveoli, or air sacs in the lungs, is caused by the infection. Breathing becomes difficult when the alveoli get blocked with fluid or pus. For example, relation of smoking with pneumonia.
When the lungs get infected, various things happen, including:
Your bronchial tubes swell (become inflamed)
Mucus and other fluids fill the air sacs of the lungs.
Types of Pneumonia
The sort of pneumonia you have is determined by where you contracted the illness.
Walking Pneumonia.
Walking pneumonia is caused by bacteria that cause milder, more gradual symptoms than other varieties of pneumonia.
Walking pneumonia is a colloquial phrase for pneumonia that isn’t severe enough to necessitate bed rest or admission to the hospital. It’s possible that you have a cold. Because the sensations are usually so light, you don’t feel compelled to remain home from work or school, so you go for a stroll.
The following are some of the symptoms of walking pneumonia:
· Moderate temperature
· A week-long dry cough
· Chills
· Chest discomfort
· A lack of appetite
Viral Pneumonia.
Pneumonia is caused by viruses, which are the second most prevalent cause. The disease is caused by a variety of viruses, including some of the same viruses that cause colds and flu, as well as the corona virus that causes COVID-19.
Virulent pneumonia has symptoms that are similar to the flu, including:
· Fever
· Chills
· Dry cough that may worsen and produce mucus
· Clogged nose
· Muscle ache
· Headache
· Tiredness
· Weakness
Bacterial Pneumonia.
Bacterial pneumonia is a bacterial illness that affects your lungs. The most common bacterium is streptococcus (pneumococcus); however other bacteria can potentially cause sickness. Along with viruses, parasites, and fungus, different forms of bacteria, as well as other pathogens, can cause pneumonia and substantial injury.
Symptoms for bacterial pneumonia
· Fever of up to 105 degrees Fahrenheit.
· Greenish, yellow, or red mucus is coughed up.
· The kinds of chills that make you shiver.
· You can’t seem to catch your breath, especially if you’re moving about a lot.
· Quite exhausted and drenched with sweat.
· Chest discomfort that is sharp or stabby, especially while coughing or taking a deep breath.
· There’s a lack of desire to eat.
· Breathing and heartbeat are both quite fast.
· Confusion is common, especially among the elderly.
· Your lips and fingernails are changing colour.
Chemical Pneumonia.
Inhaling chemical vapours or breathing in and choking on certain chemicals can cause chemical pneumonitis, which causes inflammation of the lungs and trouble breathing. Chemical pneumonia can be caused by a variety of chemicals, including liquids, gases, and microscopic particles, such as dust or fumes, often known as particulate matter.
Symptoms for chemical pneumonia are:
· Nose, eyes, lips, mouth, and throat are all red and burning.
· Cough that is dry
· Clear, yellow, or green mucus produced by a wet cough.
· Blood or frothy pink stuff in the saliva after coughing.
· Nausea or stomach ache are both possible symptoms.
· Pain in the chest
· Breathing difficulties
· Pleurisy (inflammation of the lungs) or bronchitis (inflammation of the (an inflammation of the outside covering of the lungs).
· Headache.
· Symptoms of the flu
· Weakness or a bad mood.
· Disorientation or delirium
Stages of Pneumonia
There are 4 stages of pneumonia.
Stage 1: Congestion
The lung has increased blood flow and swelling to the airways in the first stage, which begins within 24 hours of infection, but just a few bacteria or white blood cells to combat infection are present.
Stage 2: Red Hepatization
After 48 to 72 hours, it begins and lasts for 2 to 4 days. The diseased lung becomes increasingly dry, granular, and airless, with a consistency similar to that of liver. The airways in the lungs can get clogged with red cells, white cells, germs, and cellular debris.
Stage 3: Grey Hepatization
In the third stage, the debris thins and becomes more fluid-like (days 4-6); the lung accumulates more damaged red blood cells and an increase in fibrin (exudative). The formation of macrophages, a kind of big white blood cell, begins.
Stage 4: Resolution
The final stage of recuperation takes place between days 8 and 10. Cell death fluids and breakdown products are reabsorbed. Macrophages (large white blood cells) are present and assist in the removal of dead white blood cells (neutrophils). This debris may be coughed up. The function of the airways and air sacs (alveoli) in the lungs returns to normal.
Persistent pulmonary edoema can lead to chronic lung disease (such as airway narrowing or pleural adhesions).
Typical Bacterial Pneumonia
Because the appearance and natural history of certain people with pneumonia differed from those with pneumococcal infection, pneumonias were classified as either typical or atypical.
Pneumocystis pneumonia
The fungus Pneumocystis jirovecii causes Pneumocystis pneumonia (PCP), which is a deadly illness. This is a relatively common fungus. Most people’s immune systems have already fought it off by the time they are 3 or 4 years old. However, it can make those with compromised immune systems, such as those who have HIV, very ill. Pneumocystis is assumed to be spread from person to person by airborne transmission.
PCP symptoms can appear over a period of days or weeks and include 1, 6–8.
· High temperature
· Tiredness (tiredness)
· Pain in the chest
· Cough
· Breathing problems
· Chills
Pneumococcal pneumonia
Pneumococcal pneumonia begins in the upper respiratory tract and extends to the blood, lungs, middle ear, and nervous system. Because the immune system normally declines with age, being 65 or older is a major risk factor for pneumococcal pneumonia, even if you’re healthy and active. Pneumococcal pneumonia is also more likely in persons who have specific medical disorders, such as chronic heart, lung, or liver illness, or sickle cell anemia.
Pneumococcal pneumonia can strike without warning. You may have a strong shaking cold at first, followed by:
· High fever
· Tiredness
· Breathing problems.
· Chest aches, rapid breathing
· Nausea
· Vomiting
· Headache
· Cough
Streptococcus pneumonia
Streptococcus pneumonia is a gram-positive, facultative anaerobic bacterium that comes in a lancet form and has over 100 recognized serotypes. They normally occur in pairs (diplococcic), do not produce spores, and are not motile. Streptococcus pneumonia is an alpha-hemolytic bacterium, which means it can degrade red blood cells by producing hydrogen peroxide (H2O2).
Pneumonia is the most frequent Streptococcus pneumonia infection, with symptoms including fever, chills, cough, fast breathing, breathing trouble, and chest discomfort. Confusion, decreased alertness, and the previously stated symptoms, to a lesser extent, may be present in the elderly.
Smoking and Pneumonia
Community-acquired pneumonia (CAP) and invasive pneumococcal illness are both increased by active smoking.
In individuals with chronic obstructive pulmonary disease, cigarette smoking is a significant risk factor for pneumococcal pneumonia.
Streptococcus pneumonia is the bacteria that cause community-acquired pneumonia (CAP), which is most usually connected to smoking, especially in invasive pneumococcal disease and septic shock.
Researchers discovered that 9 percent of smokers brought to the hospital for pneumonia got lung cancer within a year, therefore they advise heavy smokers treated for pneumonia to get screened for lung cancer early.
People for ask
What causes pneumonia?
Pneumonia can be caused by a variety of bacteria. Bacteria and viruses, as well as fungi in the air we breathe, are the most frequent. Your body normally prevents these viruses from infecting your lungs. Even if your health is normally strong, these pathogens can occasionally overwhelm your immune system.
What are the four signs of pneumonia?
The four signs of pneumonia are
· Greenish, yellow, or even red mucus may be produced by coughing.
· Fever, perspiration, and shivering chills are all symptoms of a fever.
· Breathing problems.
· Sharp or stabbing chest pain that gets worse when you breathe deeply or cough.
What is pneumonia explained?
Pneumonia (nu-mo’ne-a) is a condition in which the air sacs in the lungs become inflamed as a result of an injury, such as an infection. Bronchopneumonia is a condition in which the airways are also affected. Pneumonia can affect one or more areas of the lungs.
What is the difference between pneumonia and pneumococcal?
Pneumonia is a lung illness, whereas pneumococcal [noo-muh-KOK-uhl] disease refers to any infection caused by Streptococcus pneumonia, often known as pneumococcus. Ear and sinus infections, as well as pneumonia and bloodstream infections, can all be caused by pneumococcal bacteria.
What are the symptoms of pneumococcal?
Symptoms of pneumococcal pneumonia are Fever, cough, shortness of breath, chest discomfort, stiff neck, disorientation, light sensitivity; joint pain, chills, ear ache, insomnia, and irritability are all symptoms of the flu. Pneumococcal illness can result in hearing loss, brain damage, and death in extreme situations.
What does pneumococcal cause?
Pneumococcal disease] is caused by bacteria (Streptococcus pneumonia) that can infect various regions of the body. When these bacteria go into the lungs, they can cause pneumonia; when they get into the circulation, they can cause sepsis; and when they get into the brain’s covering, they can induce meningitis.
When is pneumococcal vaccine recommended?
Pneumococcal immunization is recommended for all children under the age of two and adults aged 65 and up.
If you’re 65 or older and getting your first pneumococcal immunization, you’ll need two injections, one year apart. If you’ve only gotten one pneumococcal vaccine in your life, you could need another now. If you had the pneumococcal vaccination before the age of 65, you may need one or two more injections today.
What is the cure for pneumococcal pneumonia?
Most patients with mild/moderate pneumococcal pneumonia may react to oral amoxicillin, and most patients with severe pneumonia may respond to intravenous ceftriaxone, cefotaxime, or amoxicillin-clavulanic acid, dependent on current levels of penicillin and cephalosporin resistance.
How serious is pneumococcal disease?
Invasive pneumococcal disease is a potentially lethal infection that affects 10% of people. Serious consequences are more likely in the elderly and those with underlying medical issues.
Pneumococcal meningitis kills about 1 in every 12 children and 1 in every 6 older people who contract it. Those who make it may face long-term difficulties.
Is pneumonia caused by Streptococcus pneumonia?
Middle ear infections, sepsis (blood infection) in youngsters, and pneumonia in vulnerable people and the elderly are all caused by Streptococcus pneumoniae. Pneumococcal infections can be found all over the world, although they are most common in the winter and early spring.
What is Streptococcus pneumonia infection?
Respiratory droplets are inhaled (e.g. coughing, sneezing) from an infected individual spreads Streptococcus pneumonia from person to person. Why some people acquire invasive Streptococcus pneumonia and others don’t is unknown.
Where can you get Streptococcus pneumonia?
The bacterium Streptococcus pneumonia is typically found in the nose and throat. In youngsters, the elderly, and others with low immune systems, the bacterium can cause serious sickness. The majority of people who are exposed to the bacteria have no symptoms because their immune systems prevent the germs from spreading to other parts of the body.
If a person’s immune system is compromised, germs can spread from the throat to the lungs, blood, sinuses, middle ear, and brain. This might result in a serious infection.
Is Streptococcus pneumonia harmful or helpful?
Some are safe, while others are useful, and some, unfortunately, cause sickness. Others, like the ubiquitous bacteria Streptococcus pneumonia, are difficult to classify. They’re traitors who can go from nice to bad in an instant. In most cases, the bacterium lives innocuously in people’s nasal passages. It lives in the human respiratory tract as a communally organism, meaning it benefits from the human body without damaging it.
Who is at risk for Streptococcus pneumonia?
Children and certain adults are at a higher risk.
Infection may strike anyone at any time. The elderly, children under the age of two, youngsters who frequent group day-care facilities and persons with recent viral illness or underlying medical disorders are at increased risk of infection.
What antibiotics treat Streptococcus pneumonia?
Trovafloxacin is a fluoroquinolone that has been shown to be effective in vitro against Streptococcus pneumonia strains resistant to cefotaxime and ceftriaxone.
Conclusion
Pneumonia is a significant cause of death in people with severe dementia, and many of them are treated with parenteral antibiotics. Advance care planning, the patient’s cultural background, and clinical aspects of the probable pneumonia episode all influence the treatment’s intensity. In otherwise healthy people, smoking with pneumonia appears to be the single largest risk factor for pneumococcal pneumonia.